 press-releases
press-releases 
Jan. 20, 2023 – Scientists have made big strides in the fight against cancer. A person’s risk of dying of cancer in the U.S. fell by 27% in the past 2 decades, thanks in large part to researchers who continue to uncover the complex details of how cancer works and to make advances in treatment.
Now the emerging technology of 3D bioprinting – like 3D printing for the human body, using actual human cells – promises to speed up that research, by enabling scientists to develop 3D tumor models that better represent samples from patients.
The impact could be “huge,” says Y. Shrike Zhang, PhD, an assistant professor of medicine at Harvard Medical School and associate bioengineer at Brigham and Women’s Hospital, who studies 3D bioprinting. “It is not the only technology that may allow modeling of tumors in vitro, but it certainly is one of the most capable.”
Why does that matter? Because the 2D cell cultures that scientists often use now may not capture all the complexities of how cancer grows, spreads, and responds to treatment. It’s one reason why so few potential new cancer drugs – 3.4%, according to one estimate – can pass all clinical trials. Results may not carry over from the culture dish to the patient.
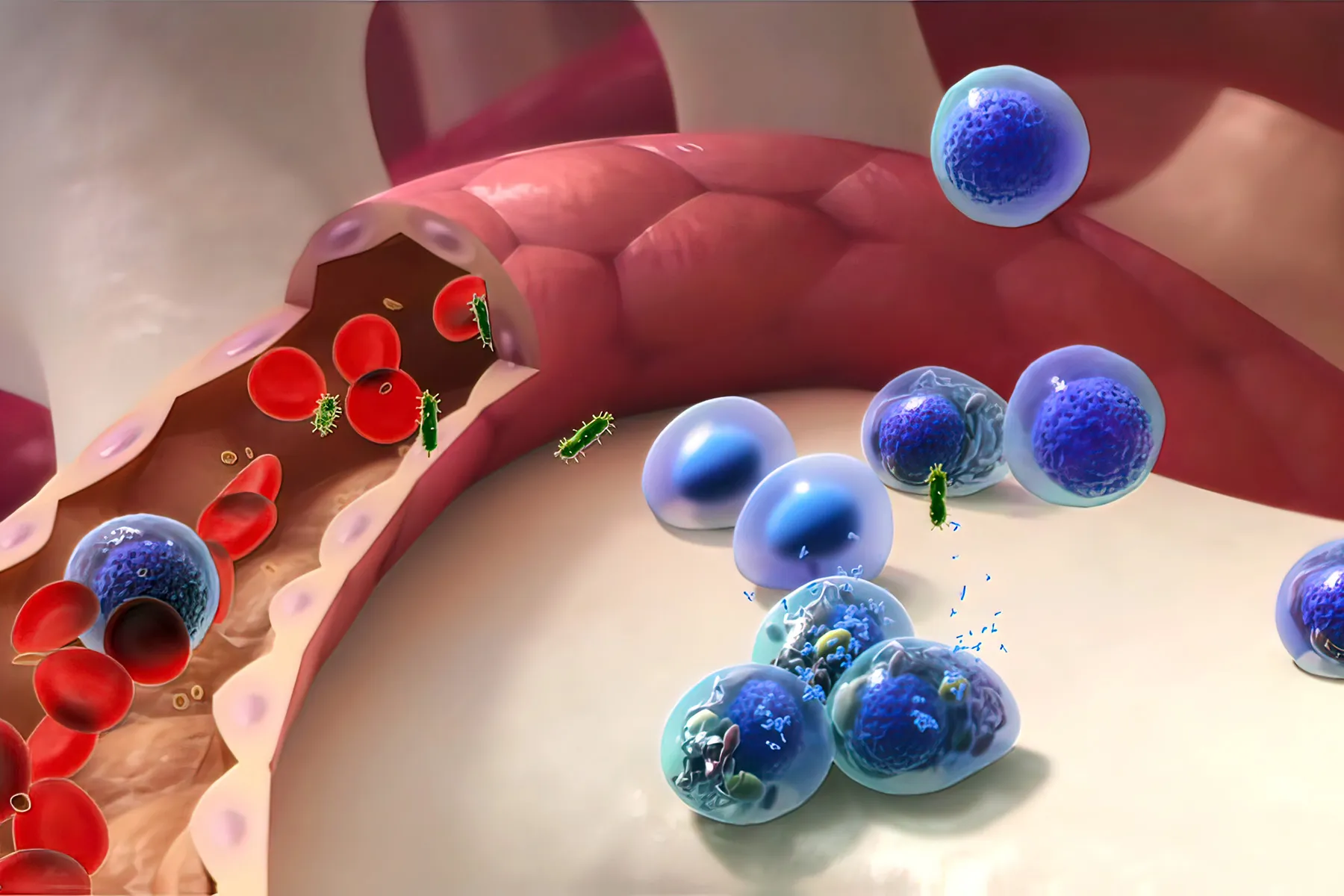
A 3D-bioprinted model, on the other hand, may be better at copying a tumor’s “microenvironment” – all the parts (cells, molecules, blood vessels) that surround a tumor.
“The tumor microenvironment plays an integral role in defining how cancer progresses,” says Madhuri Dey, a PhD candidate and researcher at Penn State University. “In-vitro 3D models are an attempt at reconstituting a [cancer] microenvironment, which sheds light on how tumors respond to chemo or immunotherapeutic treatments when they are present in a native-like microenvironment.”
Dey is the lead author of a study (funded by the National Science Foundation) in which breast cancer tumors were 3D-bioprinted and successfully treated. Unlike some previous 3D models of cancer cells, this model did a better job of imitating that microenvironment, explains Dey.
So far, “3D bioprinting of cancer models has been limited to bioprinting of individual cancer cells laden in hydrogels,” she says. But she and her colleagues developed a technique (called aspiration-assisted bioprinting) that lets them control where blood vessels are located relative to the tumor. “This model lays the foundation for studying these nuances of cancer,” Dey says.
“This is a quite cool work,” Zhang says of the Penn State study (which he was not involved in). “Vascularization is always a key component in [a] majority of the tumor types.” A model that incorporates blood vessels provides a “critical niche” to help tumor models reach their full potential in cancer research.
A 3D Printer for Your Body
Chances are you’ve heard of 3D printing and may even own (or know someone who owns) a 3D printer. The concept is like regular printing, but instead of spewing ink onto paper, a 3D printer releases layers of plastic or other materials, hundreds or thousands of times, to build an object from the ground up.
Three-dimensional bioprinting works much the same way, except those layers are made of living cells to create biological structures like skin, vessels, organs, or bone.
Bioprinting has been around since 1988. So far, it’s mainly used in research settings, such as in the field of regenerative medicine. Research is underway for ear reconstruction, nerve regeneration, and skin regeneration. The technology was also recently used to create eye tissue to help researchers study eye diseases.
The technology’s potential for use in cancer research has yet to be fully realized, Dey says. But that may be changing.
“The use of 3D-bioprinted tumor models is getting close to translations in cancer research,” says Zhang. “They are being increasingly adopted by the research field, and [the technology] has started to be explored by the pharma industry for use towards cancer drug development.”
Because bioprinting can be automated, it could allow researchers to create high-quality, complex tumor models at scale, Zhang says.
Such 3D models also have the potential to replace or reduce the use of animals in tumor drug testing, Dey notes. They “are expected to provide a more accurate drug response compared to animal models, as animal physiology does not match humans’.”
The FDA Modernization Act 2.0, a new U.S. law eliminating the requirement that drugs be tested in animals before humans, has “further paved the way for such technologies in the drug development pipeline,” Zhang says.
What if We Could Build a Custom Tumor Model for Each Patient?
Possible uses for bioprinting go beyond the lab, Dey says. Imagine if we could customize 3D tumor models based on biopsies from individual patients. Doctors could test many treatments on these patient-specific models, letting them more accurately predict how each patient would respond to different therapies. This would help doctors decide which course of treatment is best.
In Dey’s study, the 3D model was treated with chemotherapy and with immunotherapy, and it responded to both. This highlights the potential for such 3D models to reveal the body’s immune response and be used to screen therapies, Dey says.
“We hope is that in the future, this technique can be adapted in the hospital, which would speed up the course of cancer treatment,” says Dey.
To that end, she and her colleagues are now working with real breast cancer tumors removed from patients, re-creating them in the lab in 3D to use for chemo and immunotherapy screening.
24World Media does not take any responsibility of the information you see on this page. The content this page contains is from independent third-party content provider. If you have any concerns regarding the content, please free to write us here: contact@24worldmedia.com